Male fertility plays a crucial role in the success of in vitro fertilization (IVF) treatments. While much attention is often focused on female fertility, it is important to recognize the significant impact that male factors can have on the overall outcome of IVF. Understanding male fertility, its role in IVF, diagnosing fertility issues, and strategies to improve male fertility are essential in maximizing the chances of a successful IVF journey for couples.
Understanding Male Fertility
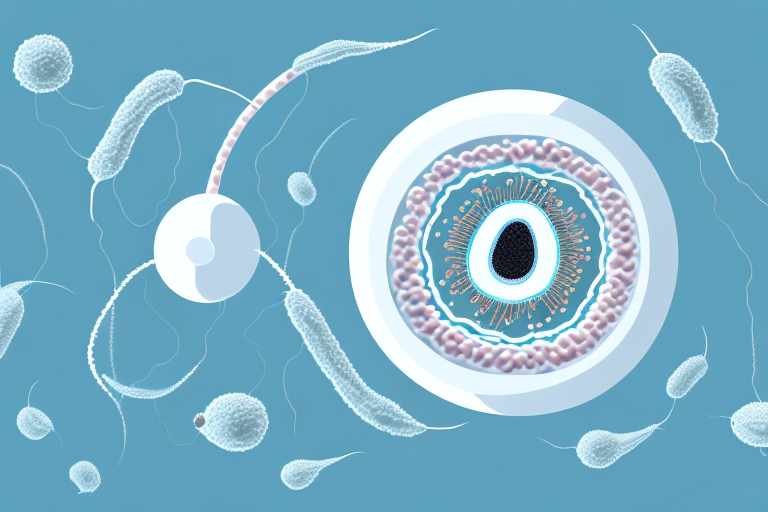
Male fertility refers to a man’s ability to impregnate a woman. It relies on the production of healthy sperm that can fertilize a woman’s egg. The process of male fertility involves multiple factors, including sperm quality, quantity, and motility. Understanding these aspects is key to comprehending how they influence IVF success.
The Basics of Male Reproductive Health
The male reproductive system consists of various organs, including the testes, epididymis, vas deferens, prostate gland, and seminal vesicles. These organs work together to produce, store, and deliver sperm. Healthy production and function of these structures are essential for male fertility and contribute to the likelihood of IVF success.
The testes, located in the scrotum, are responsible for producing sperm and testosterone. Spermatogenesis, the process of sperm production, occurs within the seminiferous tubules of the testes. The epididymis, a coiled tube located on the back of each testicle, serves as a storage and maturation site for sperm. From the epididymis, sperm travel through the vas deferens, a muscular tube that carries them to the ejaculatory ducts.
The prostate gland, situated just below the bladder, produces a fluid that nourishes and protects sperm. This fluid, along with secretions from the seminal vesicles, makes up the majority of semen. During ejaculation, the muscles in the reproductive system contract, propelling semen through the urethra and out of the penis.
Common Causes of Male Infertility
Male infertility can be caused by various factors, including hormonal imbalances, genetic conditions, physical abnormalities, and lifestyle choices. Hormonal imbalances, such as low testosterone levels, can negatively affect sperm production and quality. Testosterone, the primary male sex hormone, plays a crucial role in regulating sperm production.
Genetic conditions, such as Klinefelter syndrome, can also impact fertility. Klinefelter syndrome is a chromosomal disorder in which males have an extra X chromosome (XXY) instead of the usual XY. This condition can lead to reduced sperm production and quality, as well as other reproductive challenges.
Additionally, physical abnormalities can hinder male fertility. Varicoceles, which are enlarged veins in the scrotum, can disrupt the temperature regulation of the testes, potentially impairing sperm production. Blockages in the reproductive system, such as those caused by infections or previous surgeries, can prevent sperm from reaching the egg, resulting in infertility.
Lifestyle choices can also have a significant impact on male fertility. Smoking tobacco has been linked to decreased sperm count, motility, and morphology. Excessive alcohol consumption can disrupt hormone production and impair sperm quality. Obesity, defined as having a body mass index (BMI) of 30 or higher, can lead to hormonal imbalances and reduce fertility.
It is important to note that male fertility is a complex topic, and the factors mentioned above are just a few examples of what can influence it. Consulting with a healthcare professional specializing in reproductive medicine can provide further insight and guidance for individuals or couples seeking to understand and address male fertility concerns.
The Role of Male Fertility in IVF
Male fertility significantly affects the different stages of the IVF process, including sperm retrieval, fertilization, and embryo development.
When it comes to in vitro fertilization (IVF), the focus is often on the female partner and her reproductive health. However, it is important to recognize that male fertility plays a crucial role in the success of IVF as well. The quality of sperm used in the process can greatly impact the outcome, from fertilization to embryo development.
The Importance of Sperm Quality in IVF
Sperm quality plays a critical role in IVF success. High-quality sperm have better motility, morphology, and DNA integrity, increasing the chances of successful fertilization and embryo development. Therefore, evaluating sperm quality through semen analysis is an essential step in IVF treatment.
During semen analysis, various parameters are assessed to determine the quality of sperm. Motility refers to the sperm’s ability to move and swim towards the egg, while morphology refers to the shape and structure of the sperm. DNA integrity, on the other hand, ensures that the genetic material within the sperm is intact and capable of supporting healthy embryo development.
By analyzing these factors, fertility specialists can identify any potential issues with sperm quality and take appropriate measures to optimize the chances of successful IVF. Techniques such as sperm washing and sperm selection can be employed to ensure that only the healthiest and most viable sperm are used for fertilization.
How Male Fertility Affects Embryo Development
The quality of sperm used in IVF directly impacts the quality of embryos. Healthy sperm contribute to the development of high-quality embryos, which have a higher chance of implantation and successful pregnancy. Conversely, poor sperm quality can lead to lower-quality embryos, affecting the overall success rate of IVF.
Embryo development is a complex process that relies on the interaction between the sperm and the egg. When high-quality sperm fertilize the egg, the resulting embryo is more likely to have the necessary genetic material and cellular components for successful implantation in the uterus. On the other hand, if the sperm used in IVF has compromised quality, it can result in embryos with chromosomal abnormalities or developmental issues.
It is worth noting that male fertility factors can also impact the overall health of the embryo beyond genetic considerations. For example, certain sperm abnormalities or conditions, such as DNA fragmentation or oxidative stress, can affect the embryo’s ability to develop and thrive in the early stages of pregnancy.
Therefore, it is crucial for both partners to undergo thorough fertility evaluations before undergoing IVF. By addressing any potential male fertility issues, fertility specialists can optimize the chances of successful fertilization, embryo development, and ultimately, a healthy pregnancy.
Diagnosing Male Fertility Issues
Accurate diagnosis of male fertility issues is crucial in optimizing IVF outcomes. Medical tests and professional evaluation are essential in identifying the cause of male infertility.
When it comes to diagnosing male fertility issues, there are a variety of medical tests that can be conducted. These tests provide valuable information that helps healthcare providers determine the underlying causes of infertility. By understanding the specific factors contributing to male infertility, healthcare providers can develop personalized treatment plans that address the unique needs of each individual.
Medical Tests for Male Fertility
Various tests can assess male fertility, including semen analysis, hormone testing, genetic screening, and imaging studies.
Semen analysis is one of the most common tests used to evaluate male fertility. This test measures the quantity, quality, and movement of sperm in a semen sample. By analyzing factors such as sperm count, motility, and morphology, healthcare providers can gain insight into the overall health and function of the sperm.
Hormone testing is another important tool in diagnosing male fertility issues. Hormonal imbalances can have a significant impact on fertility, and hormone testing helps identify any abnormalities that may be affecting sperm production or function. By assessing hormone levels, healthcare providers can determine if there are any underlying hormonal issues that need to be addressed.
In some cases, genetic screening may be recommended to identify any genetic abnormalities that may contribute to infertility. Genetic factors can play a role in male fertility, and screening tests can help identify any potential genetic issues that may affect sperm production or function.
Imaging studies, such as ultrasound, can also be used to detect physical abnormalities within the reproductive system. These abnormalities may include blockages or structural issues that can hinder sperm production or delivery. By visualizing the reproductive organs, healthcare providers can identify any physical factors that may be contributing to male infertility.
Interpreting Fertility Test Results
Interpreting fertility test results should be done by a qualified healthcare provider. They can analyze the test findings and provide necessary guidance on potential treatment options.
Understanding the test results is crucial for couples undergoing IVF treatment. By comprehending the findings, couples can make informed decisions regarding their treatment plan. They can discuss the results with their healthcare provider and gain a better understanding of the potential causes of male infertility. This knowledge allows couples to explore different treatment options and make choices that are best suited to their unique situation.
It’s important to remember that diagnosing male fertility issues is a complex process that requires the expertise of healthcare professionals. By conducting thorough medical tests and interpreting the results accurately, healthcare providers can provide the necessary support and guidance to couples struggling with male infertility. With the right diagnosis and treatment plan, many couples can overcome fertility challenges and achieve their dream of starting a family.
Improving Male Fertility for IVF Success
There are several strategies that men can employ to improve their fertility and increase the chances of IVF success.
Lifestyle Changes to Boost Fertility
Making healthy lifestyle choices can significantly improve male fertility. Quitting smoking, reducing alcohol intake, maintaining a healthy weight, and exercising regularly can positively impact sperm quality and overall reproductive health. A balanced diet rich in fruits, vegetables, lean proteins, and whole grains can also support optimal sperm production and function.
Medical Treatments for Male Infertility
Depending on the underlying cause of male infertility, various medical treatments may be recommended. These can include hormone therapy, surgical interventions to correct physical abnormalities, or assisted reproductive technologies, such as intracytoplasmic sperm injection (ICSI). Consulting with a fertility specialist is crucial in determining the most suitable treatment option for individual cases.
The Psychological Impact of Male Infertility
Dealing with fertility issues can have a significant emotional toll on men. The psychological impact of male infertility should not be overlooked, as it can cause stress, anxiety, and feelings of inadequacy.
Dealing with Emotional Stress
Men should acknowledge and address their emotional well-being throughout the IVF journey. Open communication with their partner, seeking support from loved ones, and considering professional counseling or support groups can be beneficial in managing emotional stress and fostering a positive mindset during this challenging time.
Support and Resources for Men with Fertility Issues
There are various support networks and resources available for men facing fertility challenges. Online forums, support groups, and organizations specializing in male infertility can provide a safe space for men to share experiences, seek advice, and find emotional support. Seeking assistance from these resources helps men realize they are not alone in their journey.
Conclusion
Male fertility is a critical factor in IVF success. Understanding the basics of male reproductive health, common causes of male infertility, and the impact on the IVF process allows couples to make informed decisions about their treatment options. By addressing male fertility issues through medical tests, lifestyle changes, and appropriate treatments, couples can improve their chances of achieving successful IVF outcomes. It is essential to acknowledge and support the psychological well-being of men facing fertility challenges, providing the necessary resources to help them navigate this emotional journey.